What is a food allergy?
Food allergies are an immune system response to a food protein that the body mistakenly believes is harmful. When a person eats a food containing that protein, this causes the immune system to have a large reaction, triggering symptoms that can affect a person’s gastrointestinal tract, skin, breathing and/or heart.
In Australia, food allergy is estimated to affect 1-2% of adults, 4-8% of children and 10% of infants under 5 years of age (https://allergyfacts.org.au/allergy-anaphylaxis/food-allergy). Some of them will experience life-threatening allergic reactions.
Are food allergies on the rise in Australia?
Australia takes the cake as the allergy capital of the world, and according to research from the Murdoch Children’s Research Institute, has the highest published rates of food allergy in children!
Several factors have been identified by researchers as to the reason why the rates are rising:
- Modern, urban lifestyles.
- Vitamin D deficiencies – this is thought to change immune system development.
- Changing the modern diet – the gut has been altered by increases in processed foods and food manufacturing along with higher sugar diets over the last 50 years.
- Avoidance of allergens during the first phases of an infant eating solids – it is now recommended that all children, regardless of family history of allergen, are exposed to allergenic food during the first 12 months of life.
Which foods cause allergies?
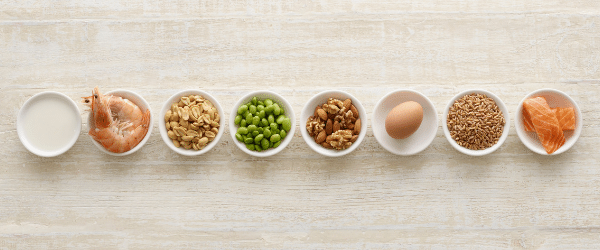
While there are more than 170 foods known to have triggered severe allergic reactions, the most common triggers of allergic reactions in childhood are:
- Egg
- Peanuts
- Tree nuts
- Cow’s Milk
Fish and shellfish allergies are most common in adulthood.
Less common (but still major) food allergies include:
- Sesame
- Soy
- Wheat
- Kiwi fruit
- Banana
- Chicken
- Mustard
- Celery
Peanut, tree nut, sesame and seafood allergies are usually lifelong.
Children often outgrow cow’s milk, egg, soy and wheat allergy at some point throughout childhood but there are a few who may continue the allergies into adulthood.
What are the symptoms of food allergies?
Some food allergies can be severe, causing life threatening reactions known as anaphylaxis.
Food allergy is the leading cause of anaphylaxis outside a hospital setting.
Allergy symptoms range from hives, rash, swelling of the mouth, vomiting to difficulty breathing, persistent dizziness, swelling of the throat and loss of consciousness and sudden collapse.
If left untreated, there is a chance these symptoms can be fatal.
Deaths from food allergies are rare. There are more fatal allergic reactions to medications and insect bites and stings than there are to foods.
Food intolerance is not life threatening, however it can cause milder reactions like digestive pain, gas, bloating and nausea.
It is important to know the difference so you can get medical attention if you or your child experiences an allergic reaction
What are the treatment options for food allergies?
Currently there is no cure for food allergies and avoidance is the only way to prevent a reaction. Even after a successful diagnosis of food allergies, avoiding trigger foods is challenging and accidental exposures are common.
Adrenaline is the first line treatment for severe allergic reactions and can be administered by an auto-injector called the EpiPen.
It is important for people with allergies to get a correct diagnosis and explore the best currently available therapies with their doctor (link). It is also important to be educated about the risk of severe allergic reactions and be prepared to treat with an EpiPen, as well as having regular reviews of an allergy action plan.
Long term actions to reduce the risk of the next generation developing food allergies include:
- Following recommendations for introduction of allergenic foods such as peanuts and eggs into the diet in infants in the first year of life
- Avoiding exposure to smoking
- Having a healthy and well-balanced diet and maintaining a healthy lifestyle
- Increasing the levels and absorption of Vitamin D
 Are food allergies different to food intolerances?
Are food allergies different to food intolerances?
Adverse reactions to foods occur in a small proportion of the population. These reactions are not the same as allergies, but may include:
- Irritable bowel symptoms, colic, bloating, diarrhoea
- Migraines, headaches, lethargy, irritability
- Rashes and swelling of the skin, asthma, stuffy or runny nose
With the processing and manufacturing of foods in modern times, added ingredients including food additives, food colourings, processing aids and extra inclusions of naturally occurring food components such as lactose and gluten can be a cause of food intolerance.
To properly diagnose a food intolerance under medical supervision and guidance, you can start by eliminating all suspect foods from the diet and reintroduce them one by one to see which food or component of food causes a reaction.
If you think your child (or yourself) has a food intolerance, it is important to seek advice and clarification from a medical practitioner since the symptoms may be related to any number of other conditions.



 Are food allergies different to food intolerances?
Are food allergies different to food intolerances?

 Causes and risk of Coronary Heart Disease
Causes and risk of Coronary Heart Disease  How do you know if you have Coronary Heart Disease?
How do you know if you have Coronary Heart Disease?  How you can prevent Coronary Heart Disease
How you can prevent Coronary Heart Disease
 2. Exercise assists in weight loss and helps prevent unhealthy weight gain
2. Exercise assists in weight loss and helps prevent unhealthy weight gain 3. Exercise reduces the risk of and helps to manage cardiovascular disease, reduce risk of heart attack, lower blood cholesterol, lower blood pressure
3. Exercise reduces the risk of and helps to manage cardiovascular disease, reduce risk of heart attack, lower blood cholesterol, lower blood pressure 4. Social interaction and exercise go hand-in-hand
4. Social interaction and exercise go hand-in-hand 5. Build strong muscles and bones
5. Build strong muscles and bones
 8. Lower the risk of falls with exercise
8. Lower the risk of falls with exercise